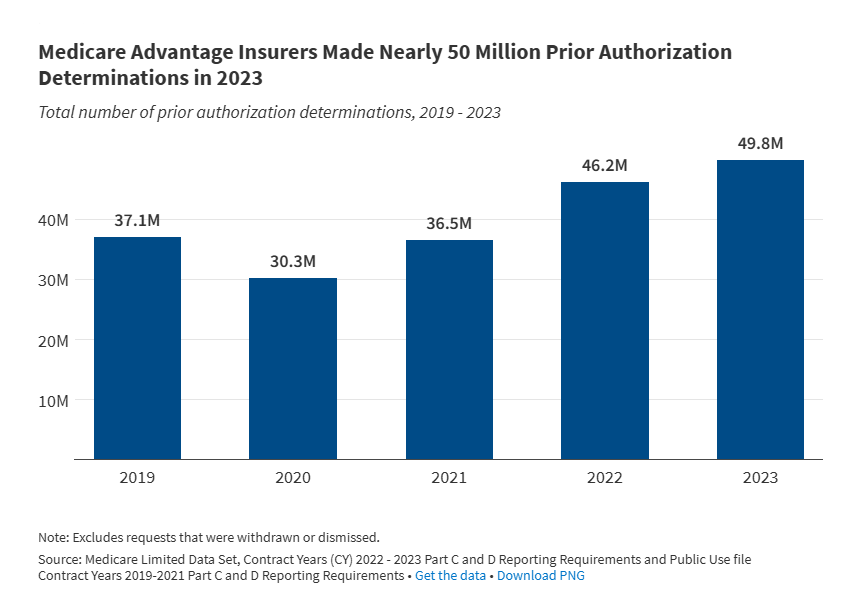
Almost all (99%) of those enrolled in Medicare Advantage require prior authorization for certain services, like inpatient hospital stays or chemotherapy. This is in contrast to traditional Medicare, which only requires prior authorization for a limited set of services. Prior authorization helps to ensure that healthcare services are necessary before coverage is provided, but can also result in administrative hassle and potential delays in care. A new analysis reveals that Medicare Advantage insurers made roughly 50 million prior authorization decisions in 2023, reflecting a steady increase since 2021.
Deepseek’s Security Risk Is A Critical Reminder For Healthcare CIOs
DeepSeek, a Chinese AI startup, sparked concern after security vulnerabilities were uncovered in their technology, exposing sensitive data from a publicly accessible database. The findings